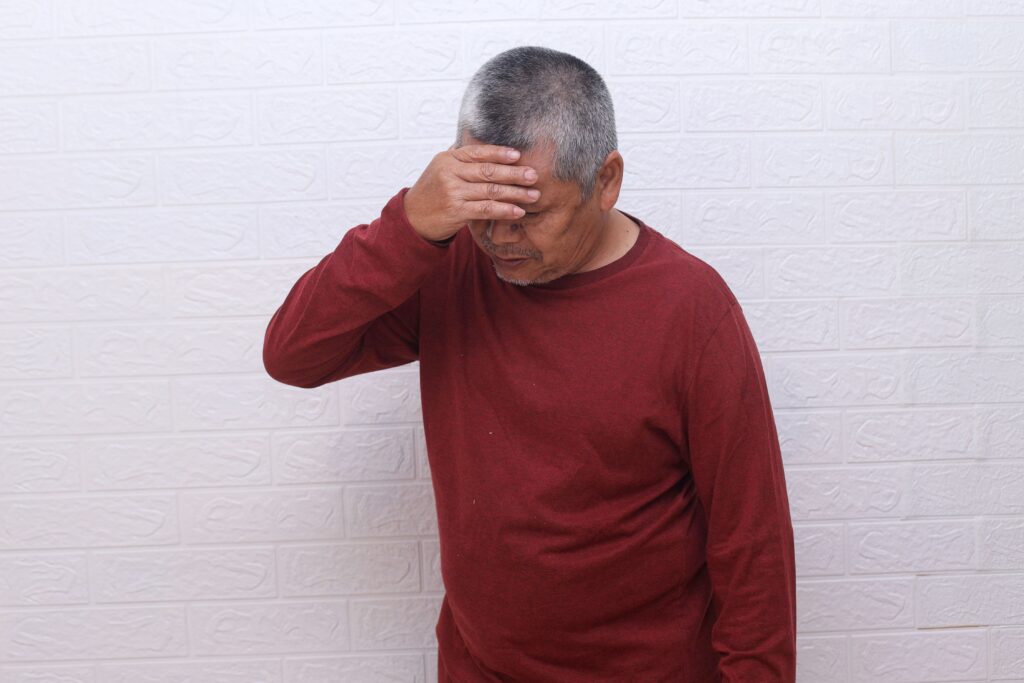
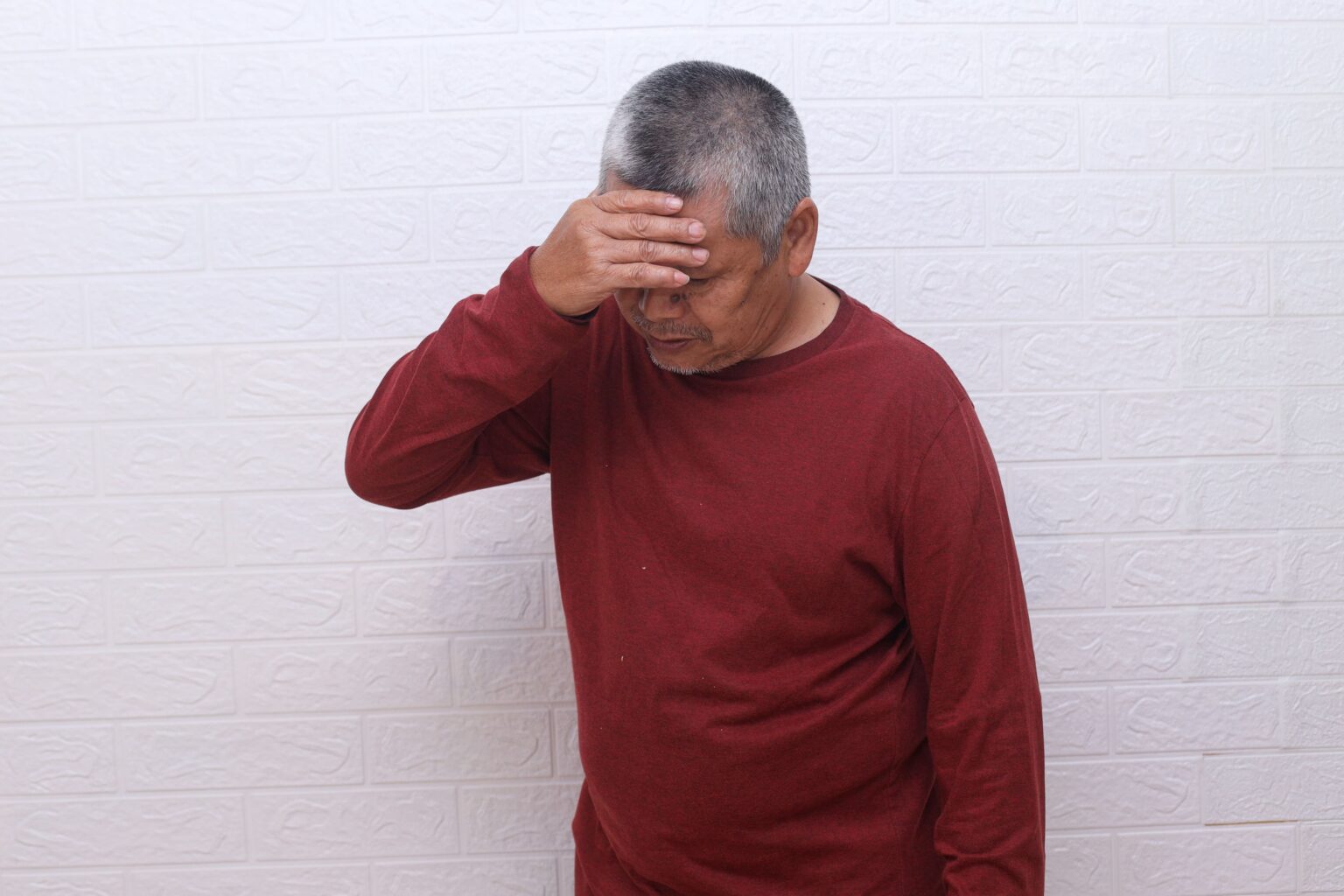
Without prompt treatment, a stroke may lead to significant brain damage. Brain cells can begin dying within minutes of oxygen deprivation (when the brain doesn’t receive enough oxygen-rich blood). As a result, the area of damage can expand rapidly. Untreated ischaemic strokes (strokes caused by blocked blood vessels) may also progress to haemorrhagic transformation, where damaged vessels begin to leak into surrounding brain tissue.
Physical complications may include:
- Paralysis (loss of movement in parts of the body)
- Muscle contractures (tightening and shortening of muscles)
- Chronic pain syndromes
Cognitive effects can range from mild memory problems to more severe difficulties with awareness and thinking. Some individuals may experience speech problems, difficulty understanding language, or loss of communication abilities.
The impact of an untreated stroke can extend beyond physical and cognitive changes. Loss of independence and reduced quality of life are possible, with some individuals requiring long-term assistance for daily activities.
Individuals who have had a stroke face an increased risk of recurrent stroke without appropriate preventive treatment. Timely treatment may help improve the chance of recovery and help reduce the risk of long-term health complications.