Head trauma specialist care involves diagnosis, treatment, and management of injuries affecting the head, brain, and related structures. The neurosurgeon evaluates the severity of the head injury, implementing treatment strategies tailored to individual needs, and monitors recovery to help prevent complications.
Specialists manage a wide spectrum of conditions, from mild concussions to severe traumatic brain injuries (TBI), which occur when an external force causes damage to the brain. Diagnostic tools are used to determine the extent of injury and guide treatment:
- Neurological examinations (checking brain and nerve function)
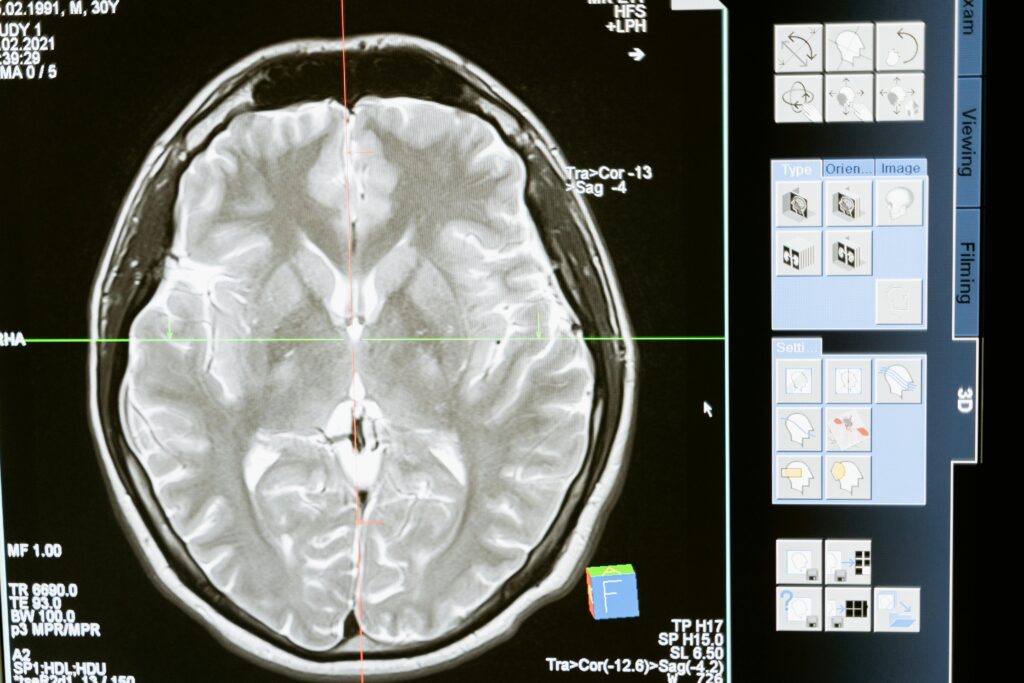
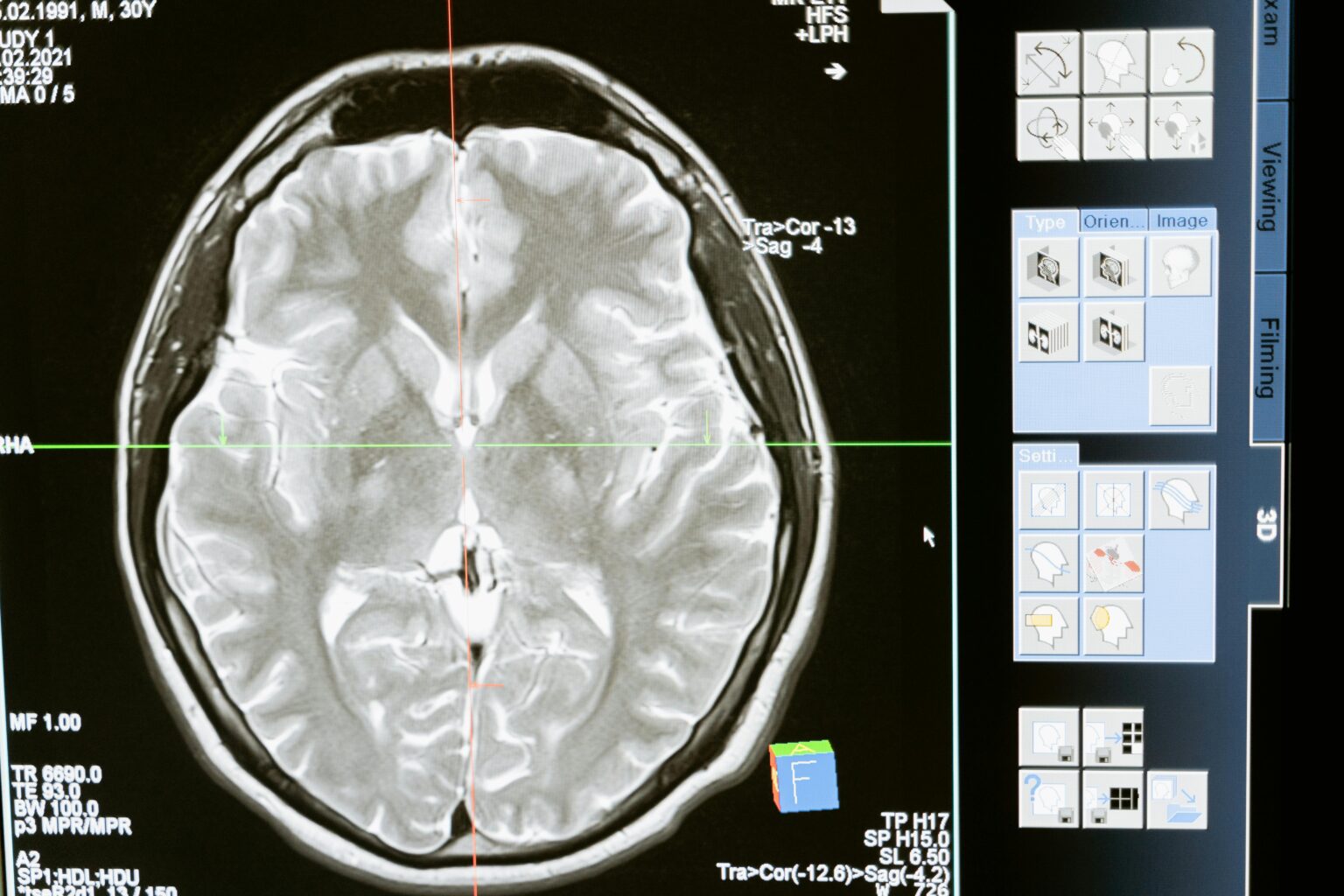
- Imaging studies (such as CT scans or MRIs)
- Cognitive assessments (evaluate thinking, memory, and concentration)
The approach to head trauma care involves both immediate treatment following injury and long-term rehabilitation planning. Specialists coordinate with multidisciplinary approaches to address multiple aspects of recovery. Treatment may range from observation and medication management to surgical intervention for severe cases.
Assessing Severity: Glasgow Coma Scale (GCS)
The GCS is commonly used to assess consciousness after head injury. Scores help determine TBI severity:
| Severity of TBI | GSC Score | Description |
|---|---|---|
| Mild | 13-15 | Minor Confusion, may be fully alert |
| Moderate | 9-12 | Decreased consciousness disorientation |
| Severe | 3-8 | Significant impairment of consciousness may rrequire intensive monitoring |
Based on the GCS, the scale is scored between 3 and 15, with being the worst and 15 being the best.